(Wimms A, Morin L, Lavergne F, Graml A, Neuzeret PC, Woehrle H, ResMed Science Centre, ResMed, Munich, Germany)
Introduction
Continuous positive airway pressure (CPAP) treatment of obstructive sleep apnoea (OSA) has proven efficacious, but adherence to therapy can be challenging. Lack of compliance is recognized as the key factor that significantly compromises the potential benefits of treatment. Currently, there is no universally-accepted definition of adequate CPAP compliance, and the cut-off points currently in use are not consistent, but it is clear that constant usage is essential.
Definition of Compliance
Compliance is defined as: ‘The extent to which the patient’s behaviour matches the prescriber’s recommendations’. Adherence, which incorporates the patients’ involvement in their treatment, is defined as: ‘The extent to which the patient’s behaviour matches agreed recommendations from the prescriber.’1 However, in the literature these terms are used interchangeably, with compliance/adherence typically referring to the consistency with which a patient uses CPAP therapy. CPAP compliance, measured as the number of hours and minutes spent breathing on the device, can be accurately determined by data stored in the CPAP device.4
There is no globally accepted definition of good CPAP compliance, and different healthcare systems have based reimbursement on a variety of cut-off points. The most widely recognized criterion for compliance is usage of a CPAP device for >4 hours per night on at least 70% of nights. The specific figure of 4 hours was based on minimal criteria for adequate sleep duration from the general sleep literature, and the 70% value was based on the author’s expert clinical opinion.11 This definition was widely accepted despite a lack of evidence that 4 hours CPAP usage was sufficient, or indeed had any health benefits compared to any other specific usage duration. Despite newer research showing that 4 hours usage may not be sufficient, along with a better understanding of the detrimental effects of sleep deprivation, the ‘4 hours for 70% of nights’ definition remains in common use today.17
Benefits of CPAP Treatment
Untreated OSA has been linked with a number of cardiovascular complications, including hypertension, coronary artery disease, congestive heart failure, cardiac arrhythmias, stroke, and even death.18 In addition to cardiovascular morbidity and mortality, untreated OSA is associated with multiple other negative effects, including excessive daytime sleepiness, reduced cognitive function (e.g. alertness, motor function, recall ability) and poor quality of life.19
CPAP treatment has been shown to decrease elevated blood pressure, improve cardiovascular disease outcomes, and reduce the risk of cardiovascular fatal and non-fatal events.20-22 CPAP treatment also eliminates excessive daytime sleepiness, improves quality of life, and restores cognitive function to normal levels.19 Although many large studies have looked at the summative benefits of CPAP treatment, it has only been recently that researchers have attempted to assess the dose-response relationship for these benefits and to understand exactly what level of compliance is required for patients to obtain the optimal health benefits of CPAP across different areas.
Cardiovascular Morbidity and Mortality
It has been suggested that non-compliance with CPAP has a greater effect on mortality than smoking as a result of the serious cardiovascular morbidity and mortality associated with untreated OSA.23
Improvements in long-term survival with CPAP treatment have been reported in different cohorts of patients with OSA. In one study conducted in 385 males, those with severe untreated OSA had higher mortality rates than those with the same OSA severity who were successfully treated with CPAP.24 Another trial in 449 patients showed that treating OSA reduced the risk of fatal and non-fatal cardiovascular events by 64%.22
Barbe and colleagues studied the effects of CPAP on hypertension and cardiovascular events in a group of 723 non-sleepy OSA patients. No significant differences were found between the CPAP and control groups, however a post-hoc analysis of randomized clinical trial data suggested that CPAP treatment might reduce the incidence of hypertension or cardiovascular events in patients who were adherent to therapy for ≥4 hours per night.3 Studies analysing the dose-response relationship between CPAP therapy and cardiovascular mortality have also found evidence that increased usage correlates with survival rates, with a significant difference in 5-year survival between those using CPAP for a mean of <1 hour per day compared with those using CPAP for 1–6 or >6 hours per day.2
Excessive Daytime Sleepiness
It is widely accepted that CPAP significantly reduces daytime sleepiness in patients with OSA. Data from a meta-analysis showed that CPAP reduced the Epworth Sleepiness Scale (ESS) score by an average of 2.9 points more than a placebo treatment in patients with OSA.30 In addition, there appears to be a clear relationship between the effectiveness of CPAP therapy and hours of use.14 Studies show a linear CPAP usage versus outcome relationship for objective and subjective sleepiness measures, in which improvements were seen after as little as 2-3 hours use, and which flattened out at CPAP use of 7 hours per night.15 Other studies have found that subjective sleepiness improves even at nightly CPAP usage levels as low as 2.5 hours13 or 4 hours,10 but that more hours of use are consistent with improved sleepiness. Data from a placebo-controlled trial showed that ≥5 hours CPAP usage per night was required to restore sleepiness and fatigue to normal levels, and that greater improvements were seen with increased CPAP use.12
Cognitive Function and Quality of Life
CPAP therapy is associated with improvements in memory and daily functioning. Return of these activities to normal levels can be seen after use of CPAP for >6 and 7.5 hours per night, respectively.31 The improvement in daily functioning may also be attributed to the longer sleeping period which patients were able to achieve by using CPAP therapy. Antic et al found that greater improvements in verbal memory and executive function were seen as CPAP usage increased.14 The results of a similar trial suggested that OSA patients with memory impairment who used CPAP treatment for an average of 6 hours per night for 3 months were nearly eight times more likely to demonstrate memory abilities in the clinically normal range compared with those who used CPAP for ≤2 hours per night over the same period.16
Withdrawal of CPAP
Not only is increasing average CPAP usage important, but consistent nightly use of CPAP may be equally as important. Studies have demonstrated that withdrawal of CPAP for even one night can have negative impacts on daytime sleepiness and driving ability.4, 32 Moreover, CPAP withdrawal for two weeks resulted in a rapid recurrence of apneic events and subjective daytime sleepiness, impaired endothelial function, increased urinary catecholamines and significant increases in blood pressure.33 Morning systolic BP increased 8.5 mmHg; (95% CI, +1.7, +15.3 mm Hg; P = 0.016), morning diastolic BP increased 6.9 mmHg (95% CI, +1.9, +11.9 mm Hg; P = 0.008), and morning heart rate was also significantly increased by an average of 6.3bpm.33 CPAP withdrawal of 2 weeks in a similar study resulted in a significant increase in the length of cardiac repolarization (QT(c), TpTe(c) intervals in the withdrawal arm compared to the treatment arm (mean difference between groups 21.4 ms, 11.3-1.6 ms, p < 0.001 and 14.4 ms, 7.2-21.5 ms, p < 0.001) which the authors stipulated may provide a possible mechanistic link between untreated OSA, and cardiac dysrhythmias, and thus sudden cardiac death.34
Economic Aspects of Compliance
Patients with untreated OSA utilize medical services and use medicines significantly more often than those without OSA.35 Untreated OSA patients are estimated to cost the UK NHS £10,645 per year.36 It has been estimated that untreated OSA patients in Europe have a 2 fold increase in medical expenses,37 and Kapur et al found that untreated OSA patients in the US had an average annual medical cost of $2720 compared with $1384 for matched controls. The authors also found that the severity of the disease was linked to an increasing medical cost. This untreated OSA was estimated to cost the US an additional $3.4 billion in medical costs.38 However when also considering the effects of the disease on fatigue, cognitive functioning, workplace performance, occupational injury, and vehicle accidents, the socio-economic costs are immense, running high into the billions.35,39 Treating OSA with CPAP has shown to decrease these excessive medical costs, and is a cost-effective way to manage the disease.37,39
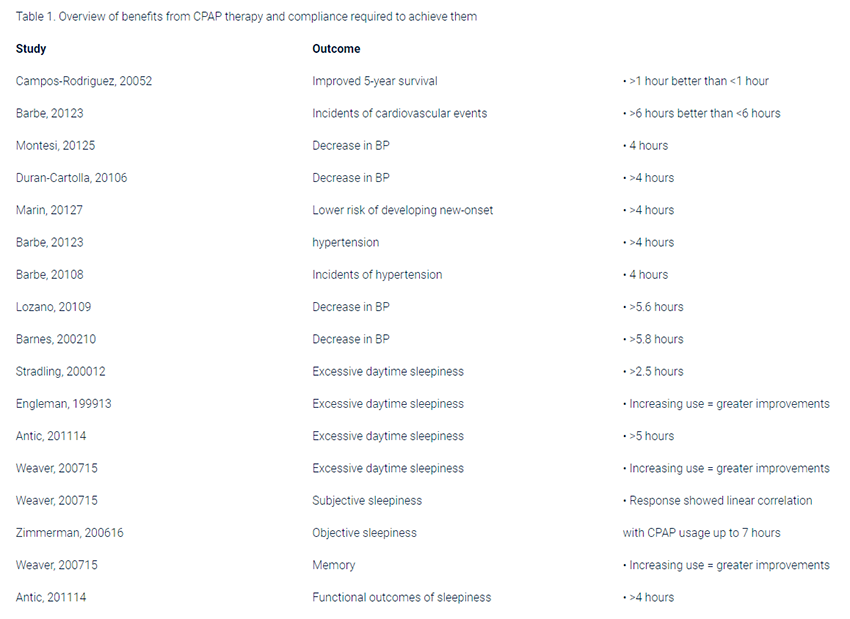
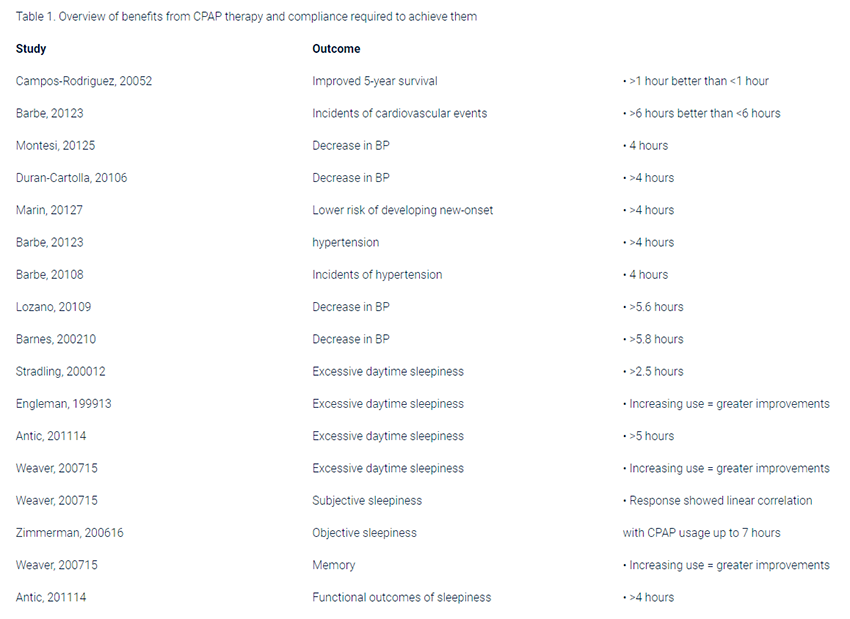
Dose-response benefits of CPAP
A summary of the dose-response benefits of CPAP therapy is shown in Table 1. The literature relating to cardiovascular fatal and non-fatal events is scarce, however current knowledge indicates that even as little as 1 hour CPAP usage can improve outcomes, with more significant improvements being seen in over 4 and 6 hours usage. Reductions in BP have been studied more frequently, with literature from 6 studies concluding that patients need to use CPAP for at least 4 hours per night to see improvements, while higher usage of more than five and a half hours leads to more pronounced blood pressure drops. Excessive daytime sleepiness appears to improve with as little as 2.5 hours per night, with multiple studies supporting a linear dose-response relationship. Studies show that cognitive functions including memory, functional outcomes of sleepiness and executive function may require at least 6 hours before improvements are seen.
Conclusion
Compliance to CPAP is the key factor required to gain the health benefits associated with treating obstructive sleep apnoea. Longer CPAP usage has been shown to improve survival, cardiovascular events, blood pressure, excessive daytime sleepiness, cognitive function, and quality of life. Increasingly research is showing that while any CPAP usage is better than no usage, the greatest improvements are correlated with the most hours of use. Healthcare systems are burdened with billions of dollars in costs associated with untreated OSA which could be saved each year if CPAP compliance was improved.
Factors which are associated with changes in patient compliance, as well as techniques for improving patient compliance can be found in Wimms et al Improving CPAP Compliance.40
If you are having issues with your CPAP compliance, please contact CPAP Club today for assistance.
References:
1. E. S. WHO Adherence Meeting Report, Geneva. World Health Organization 2001.
2. Campos-Rodriguez F, Pena-Grinan N, Reyes-Nunez N, et al. Mortality in obstructive sleep apnoea-hypopnea patients treated with positive airway pressure. Chest 2005;128:624-33.
3. Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnoea: a randomized controlled trial. JAMA 2012;307:2161-8.
4. Schwab RJ, Badr SM, Epstein LJ, et al. An Official American Thoracic Society Statement: Continuous Positive Airway Pressure Adherence Tracking Systems.
5. The Optimal Monitoring Strategies and Outcome Measures in Adults. American Journal of Respiratory and Critical Care Medicine 2013;188:613-20.
6. Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2012;8:587-96.
7. Duran-Cantolla J, Aizpuru F, Montserrat JM, et al. Continuous positive airway pressure as treatment for systemic hypertension in people with obstructiv sleep apnoea: randomised controlled trial. BMJ 2010;341:c5991.
8. Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnoea and risk of hypertension. JAMA 2012;307:2169-76.
9. Barbe F, Duran-Cantolla J, Capote F, et al. Long-term effect of continuous positive airway pressure in hypertensive patients with sleep apnoea. American journal of respiratory and critical care medicine 2010;181:718-26.
10. Lozano L, Tovar JL, Sampol G, et al. Continuous positive airway pressure treatment in sleep apnoea patients with resistant hypertension: a randomized, controlled trial. Journal of hypertension 2010;28:2161-8.
11. Barnes M, Houston D, Worsnop CJ, et al. A randomized controlled trial of continuous positive airway pressure in mild obstructive sleep apnoea. American journal of respiratory and critical care medicine 2002;165:773-80.
12. Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnoea. The American review of respiratory disease 1993;147:887-95.
13. Stradling JR, Davies RJ. Is more NCPAP better? Sleep 2000;23 Suppl 4:S150-3.
14. Engleman HM, Kingshott RN, Wraith PK, Mackay TW, Deary IJ, Douglas NJ. Randomized placebo-controlled crossover trial of continuous positive airway pressure for mild sleep apnoea/Hypopnea syndrome. American journal of respiratory and critical care medicine 1999;159:461-7.
15. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep 2011;34:111-9.
16. Weaver TE, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 2007;30:711-9.
17. Zimmerman ME, Arnedt JT, Stanchina M, Millman RP, Aloia MS. Normalization of memory performance and positive airway pressure adherence in memory impaired patients with obstructive sleep apnoea. Chest 2006;130:1772-8.
18. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep medicine reviews 2011;15:343-56.
19. Shahar E, Whitney CW, Redline S, et al. Sleepdisordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. American journal of respiratory and critical care medicine 2001;163:19-25.
20. Engleman HM, Douglas NJ. Sleep. 4: Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax 2004;59:618-22.
21. Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005;365:1046-53.
22. Haentjens P, Van Meerhaeghe A, Moscariello A, et al. The impact of continuous positive airway pressure on blood pressure in patients with obstructive sleep apnoea syndrome: evidence from a meta-analysis of placebo-controlled randomized trials. Archives of internal medicine 2007;167:757-64.
23. Buchner NJ, Sanner BM, Borgel J, Rump LC. Continuous positive airway pressure treatment of mild to moderate obstructive sleep apnoea reduces cardiovascular risk. American journal of respiratory and critical care medicine 2007;176:1274-80.
24. Yegneswaran B, Shapiro C. Which is the greater sin? Continuing to smoke or non-compliance with CPAP therapy? Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine 2011;7:315-6.
25. He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnoea index in obstructive sleep apnoea. Experience in 385 male patients. Chest 1988;94:9-14.
26. Silverberg DS, Iaina A, Oksenberg A. Treating obstructive sleep apnoea improves essential hypertension and quality of life. Am Fam Physician 2002;65:229-36.
27. Pedrosa RP, Drager LF, Gonzaga CC, et al. Obstructive sleep apnoea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension 2011;58:811-7.
28. Nieto FJ, Young TB, Lind BK, et al. Association of sleepdisordered breathing, sleep apnoea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000;283:1829-36.
29. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. The New England journal of medicine 2000;342:1378-84.
30. Chobanian AV, Bakris GL, Black HR, et al. Seventhreport of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-52.
31. Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnoea: results of a meta-analysis. Archives of internal medicine 2003;163:565-71.
32. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res 2010;131:245-58.
33. Kribbs NB, Pack AI, Kline LR, et al. Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnoea. Am Rev Respir Dis 1993;147:1162-8.
34. Kohler M, Stoewhas AC, Ayers L, et al. Effects of continuous positive airway pressure therapy withdrawal in patients with obstructive sleep apnoea: a randomized controlled trial. American journal of respiratory and critical care medicine 2011;184:1192-9.
35. Rossi VA, Stoewhas AC, Camen G, et al. The effects of continuous positive airway pressure therapy withdrawal on cardiac repolarization: data from a randomized controlled trial. European heart journal 2012;33:2206-12.
36. Jennum P, Kjellberg J. Health, social and economical consequences of sleep-disordered breathing: a controlled national study. Thorax 2011;66:560-6.
37. Guest JF, Helter MT, Morga A, Stradling JR. Costeffectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax 2008;63:860-5.
38. Wittmann V, Rodenstein DO. Health care costs and the sleep apnoea syndrome. Sleep medicine reviews 2004;8:269-79.
39. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnoea. Sleep 1999;22:749-55.
40. AlGhanim N, Comondore VR, Fleetham J, Marra CA, Ayas NT. The economic impact of obstructive sleep apnoea. Lung 2008;186:7-12.
41. Wimms AJ. Improving CPAP Compliance. ResMed White Paper 2013.
 The Importance of Regular CPAP Treatment for Sleep Apnea
The Importance of Regular CPAP Treatment for Sleep Apnea